Discover the key differences between atrial fibrillation and ventricular fibrillation, including symptoms, risks, and treatment options for each condition.
The Basics: What Are Atrial Fibrillation and Ventricular Fibrillation?
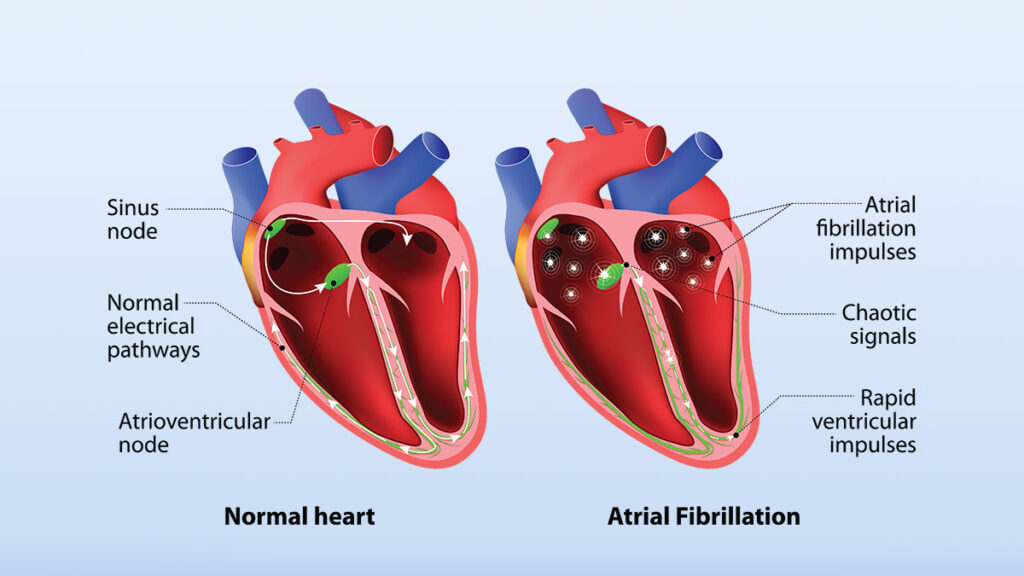
Both atrial fibrillation (AFib) and ventricular fibrillation (VFib) are types of arrhythmias, but they differ significantly in their origin, symptoms, and risks. AFib originates in the atria—the heart’s upper chambers—and causes rapid, irregular electrical signals. VFib, on the other hand, arises in the ventricles—the lower chambers—and leads to a chaotic quivering of the heart that prevents effective blood pumping and can be fatal within minutes if untreated.
Understanding these distinctions is essential, as AFib is generally a manageable chronic condition, whereas VFib is a medical emergency requiring immediate intervention.
Atrial Fibrillation: An Overview
AFib is the most common sustained arrhythmia, affecting millions worldwide. It is characterized by an erratic and rapid heartbeat that disrupts the heart’s ability to pump blood efficiently. While it can lead to serious complications, such as stroke and heart failure, AFib itself is not immediately life-threatening.
Common Symptoms of AFib:
- Palpitations or a racing heart
- Fatigue or weakness
- Shortness of breath
- Dizziness or lightheadedness
- Chest discomfort
Risk Factors for AFib:
- Advanced age
- High blood pressure (hypertension)
- Heart disease or heart failure
- Obesity
- Sleep apnea
- Excessive alcohol or caffeine intake
Complications of AFib:
The most significant complication of AFib is stroke. Blood pooling in the atria due to erratic contractions can lead to clot formation. If a clot travels to the brain, it can cause a stroke. Anticoagulation therapy is a cornerstone of AFib management to mitigate this risk.
Ventricular Fibrillation: A Closer Look
VFib is a life-threatening arrhythmia where the ventricles quiver instead of pumping blood. This results in a sudden loss of circulation, leading to cardiac arrest. VFib requires immediate treatment, typically with defibrillation, to restore a normal rhythm and prevent death.
Common Symptoms of VFib:
- Sudden collapse or loss of consciousness
- No detectable pulse or heartbeat
- Rapid progression to cardiac arrest
Risk Factors for VFib:
- Previous heart attack (myocardial infarction)
- Coronary artery disease
- Cardiomyopathy
- Severe electrolyte imbalances
- Genetic predispositions, such as long QT syndrome
Complications of VFib:
The primary risk of VFib is sudden cardiac death. Without immediate intervention, such as defibrillation or CPR, VFib is fatal. Survivors of VFib often require advanced treatments, such as implantable cardioverter-defibrillators (ICDs), to prevent recurrence.
Key Differences Between AFib and VFib
Atrial fibrillation and ventricular fibrillation are distinct in their origin, symptoms, and outcomes. AFib originates in the atria and is characterized by an irregular but usually non-fatal rhythm. It primarily increases the risk of stroke due to clot formation in the atria. In contrast, VFib originates in the ventricles and is defined by chaotic, ineffective contractions that result in a complete loss of circulation, making it a medical emergency.
While AFib symptoms include palpitations, fatigue, and shortness of breath, VFib often presents as sudden collapse or cardiac arrest with no preceding warning signs. Treatment goals also differ: AFib focuses on stroke prevention and rhythm management, while VFib demands immediate defibrillation and long-term prevention strategies, such as ICD implantation.
Treatment Options for AFib and VFib
The approaches to treating AFib and VFib vary widely due to the differences in urgency and underlying mechanisms.
AFib Treatment:
Medications: Medications are often the cornerstone of AFib management. Rate control medications, such as beta-blockers or calcium channel blockers, help to slow the heart rate, while rhythm control medications, like antiarrhythmics such as amiodarone, aim to restore and maintain a regular heartbeat. Anticoagulants, including warfarin and newer oral anticoagulants (NOACs), are prescribed to reduce the risk of stroke, which is a major complication of AFib.
Catheter Ablation: This minimally invasive procedure isolates and targets the areas in the atria causing erratic electrical signals. Catheter ablation is particularly effective for patients who do not respond to medications or continue to experience significant symptoms despite other treatments.
Cardioversion: Cardioversion is a procedure used to reset the heart’s rhythm to normal. This can be performed electrically, by delivering a controlled shock to the heart, or chemically, using specific medications. It is often used in acute cases to stabilize patients quickly.
Lifestyle Modifications: Addressing risk factors is an essential component of managing AFib. Patients are encouraged to adopt heart-healthy behaviors, such as maintaining a balanced diet, managing blood pressure, reducing alcohol and caffeine intake, and treating underlying conditions like sleep apnea and obesity to improve long-term outcomes.
VFib Treatment:
Emergency Management: Immediate defibrillation is the most critical step in managing ventricular fibrillation. This procedure delivers a controlled electrical shock to the heart to restore its normal rhythm. In the absence of immediate defibrillation access, cardiopulmonary resuscitation (CPR) is essential to maintain circulation and oxygen delivery to vital organs until defibrillation can be performed.
Long-Term Prevention: For patients who survive an episode of VFib or are at risk of recurrence, implantable cardioverter-defibrillators (ICDs) are often recommended. These devices continuously monitor heart rhythms and deliver life-saving shocks if a dangerous arrhythmia occurs. Medications, such as beta-blockers or antiarrhythmics like amiodarone, are also used to reduce the risk of future VFib episodes and to support overall heart rhythm stability.
Addressing Underlying Causes: Treating the root causes of VFib is crucial for preventing additional episodes. This includes managing coronary artery disease with procedures like angioplasty or bypass surgery, correcting severe electrolyte imbalances, and addressing genetic conditions such as long QT syndrome. Comprehensive care helps mitigate triggers and improve long-term outcomes.
Final Thoughts
Atrial fibrillation and ventricular fibrillation are both serious arrhythmias, but they differ significantly in their causes, symptoms, and treatment strategies. AFib, while generally not life-threatening, requires careful management to prevent stroke and improve quality of life. VFib, however, is a medical emergency that demands immediate intervention to prevent sudden cardiac death. Understanding these differences is essential for effective treatment and patient education. If you experience symptoms of arrhythmia, schedule a consultation with Dr. Adam Budzikowski for expert evaluation and guidance.
A Riley Publication
Medically Reviewed By: Adam Budzikowski, MD, PhD