Could CRT devices transform your heart health? Explore the benefits of this advanced treatment for heart failure.
Heart failure is a chronic, progressive condition that affects millions of people worldwide, significantly impacting their quality of life. For many patients, Cardiac Resynchronization Therapy (CRT) represents a major breakthrough, offering a proven way to improve heart function and manage symptoms. By restoring the coordinated contraction of the heart’s chambers, CRT devices help the heart pump more efficiently, reducing symptoms and improving overall outcomes.
This article takes a closer look at how CRT devices work, who they benefit, and what patients can expect from the treatment process.
What is Cardiac Resynchronization Therapy (CRT)?
Cardiac Resynchronization Therapy involves the use of specialized implantable devices, like CRT pacemakers (CRT-P)or CRT defibrillators (CRT-D), to treat heart failure patients who experience dyssynchrony, or uncoordinated beating, of the heart’s chambers. This dyssynchrony occurs when the electrical impulses controlling the heart’s contraction are delayed or blocked, causing the left ventricle—the heart’s main pumping chamber—to beat out of sync with the right ventricle.
CRT devices address this issue by delivering precisely timed electrical impulses to both ventricles, helping them contract together in a more synchronized manner. This improves the heart’s ability to pump blood efficiently throughout the body, easing heart failure symptoms and enhancing quality of life.
How CRT Devices Work
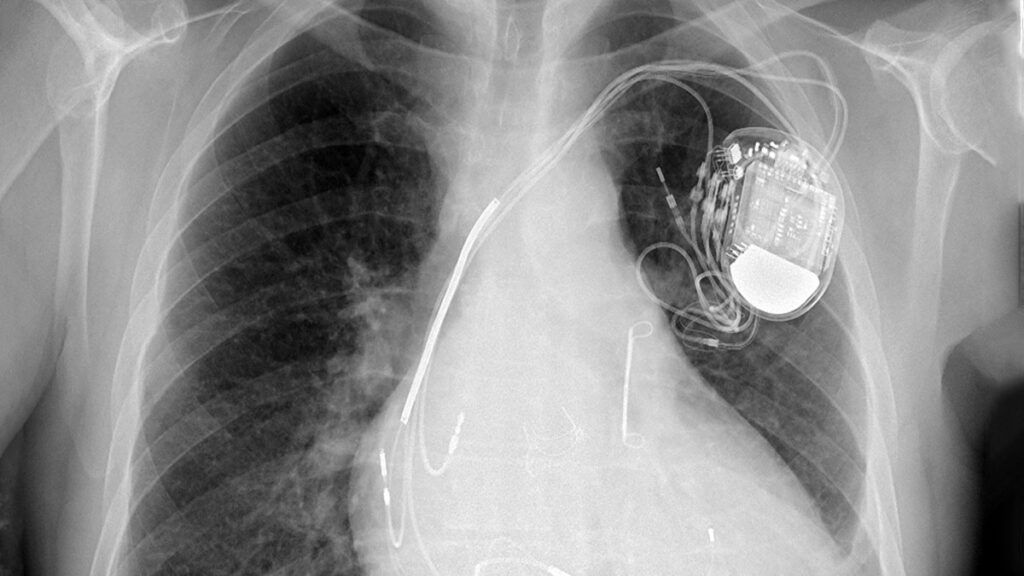
A CRT device operates similarly to a traditional pacemaker but with enhanced capabilities tailored for heart failure patients. It consists of the following components:
- The Pulse Generator is a small, battery-powered unit implanted under the skin, typically near the collarbone. It acts as the “brain” of the system, generating electrical impulses to regulate the heart’s rhythm.
- Leads are thin, insulated wires that deliver electrical signals to specific areas of the heart. CRT devices have three leads: one for the right atrium, one for the right ventricle, and a third placed near the left ventricle via the coronary sinus (CS). In some cases, Conduction System Pacing (CSP), which involves LV lead placement in areas like the His bundle or left bundle branch, is considered an alternative approach to optimize synchronization. While CSP offers promising outcomes, it is typically treated as a separate discussion point due to its distinct technique and evolving role in CRT.
- Electrodes are located at the ends of the leads, monitoring the heart’s electrical activity and delivering impulses as needed to synchronize contractions.
The Synchronization Process
When the CRT device detects an irregular rhythm or delayed electrical activation, it sends electrical signals to both ventricles simultaneously. This “resynchronization” ensures the heart’s chambers beat in unison, optimizing the pumping action and improving overall cardiac output.
Who Can Benefit from CRT?
CRT is specifically recommended for heart failure patients who meet certain criteria, including:
- Reduced Ejection Fraction (HFrEF): Patients with heart failure and reduced left ventricular ejection fraction (typically ≤35%).
- Ventricular Dyssynchrony: Evidence of uncoordinated ventricular contraction, often seen on an electrocardiogram (ECG) as a prolonged QRS duration (≥130 milliseconds).
- Heart Failure Symptoms: Patients classified as NYHA Class II, III, or IV with moderate to severe heart failure symptoms despite optimal medical therapy.
- Left Bundle Branch Block (LBBB): Patients with LBBB tend to benefit most from CRT, as this electrical disturbance contributes significantly to dyssynchrony.
Why CRT Matters
For eligible patients, Cardiac Resynchronization Therapy (CRT) has been shown to deliver significant benefits. By restoring synchronized ventricular contractions, CRT enhances cardiac output and reduces strain on the heart, ultimately improving overall heart function. Patients often experience a reduction in symptoms such as shortness of breath, fatigue, and swelling, which are common in heart failure. This symptom relief leads to an enhanced quality of life, allowing individuals to engage in greater activity levels and return to their normal daily routines.
In addition to symptom management, CRT plays a critical role in reducing hospitalizations caused by heart failure exacerbations. By improving the heart’s efficiency, the therapy helps stabilize patients and decreases the need for recurrent hospital admissions. Furthermore, studies have demonstrated that CRT significantly increases long-term survival rates for patients with advanced heart failure, making it a cornerstone treatment for improving both longevity and quality of life in this population.
The CRT Implantation Procedure
Before the Procedure
Patients undergo a thorough evaluation to confirm CRT candidacy, including:
- Echocardiogram to assess heart structure and function.
- ECG to analyze electrical activity and detect dyssynchrony.
- Blood Tests and imaging studies to ensure overall readiness for implantation.
During the Procedure
CRT device implantation is a minimally invasive procedure performed under local anesthesia and light sedation.
- Lead Placement: Using X-ray guidance, the doctor threads three leads through a vein into the right atrium, right ventricle, and near the left ventricle via the coronary sinus.
- Device Connection: The leads are connected to the CRT device, which is placed in a small pocket under the skin near the collarbone.
- Testing: The device is tested to ensure proper placement and synchronization of the ventricles.
The procedure typically lasts 2–3 hours, and most patients are discharged the same or next day.
Recovery and Long-Term Care
Immediate Recovery
Following the procedure, patients are closely observed for a few hours to ensure the device is functioning properly and that no complications arise. Careful monitoring helps confirm the success of the implantation and provides reassurance for the patient. Wound care is equally important during this stage. The incision site should be kept clean and dry to prevent infection, and patients are advised to avoid heavy lifting or strenuous activity for at least 4–6 weeks to allow proper healing. It is crucial that patients adhere to the directions provided by the physician overseeing their aftercare.
Follow-Up and Device Adjustments
Regular follow-up appointments are essential for ensuring the long-term effectiveness of the CRT device. During these visits, the device settings are fine-tuned to optimize synchronization and improve heart function. Ongoing monitoring is also performed to evaluate device performance, which may include remote monitoring to allow doctors to track heart function and CRT activity from the patient’s home.
Lifestyle Adjustments
Gradually returning to daily activities is encouraged, as CRT significantly improves exercise tolerance and overall stamina. Patients are advised to adopt a heart-healthy lifestyle, including following a low-sodium diet, adhering to prescribed medications, and engaging in regular physical activity tailored to their abilities. Additionally, patients should avoid strong magnetic fields and inform airport security personnel about their CRT device to prevent potential interference during scans. Similarly, providers should be informed of a patient’s device prior to any surgeries or imaging so the necessary programming can be coordinated. These precautions and adjustments help ensure the device functions optimally and support a smooth return to an active, fulfilling life.
Addressing Limitations and Risks
While CRT is highly effective, it may not benefit all patients equally. Potential limitations include:
- Device Non-Response: Approximately 20–30% of patients may not experience significant improvements, often due to individual heart anatomy or electrical patterns.
- Infection or Bleeding: Complications at the implantation site are rare but possible.
- Lead Displacement: Leads may shift over time, requiring repositioning or replacement.
- Coronary Sinus Dissection: During lead placement in the coronary sinus, there is a small risk of dissection, which can complicate successful lead positioning. Careful imaging and operator experience are critical for minimizing this risk.
Close follow-up with a cardiac specialist helps minimize these risks and ensures the best possible outcomes.
Conclusion
Cardiac Resynchronization Therapy (CRT) is a transformative treatment for heart failure patients experiencing ventricular dyssynchrony. By restoring the coordinated function of the heart’s chambers, CRT devices improve heart function, reduce symptoms, and enhance overall quality of life.
For individuals with advanced heart failure, CRT represents a critical step toward better health and a more active lifestyle. If you or a loved one has been diagnosed with heart failure and are considering CRT, consulting a cardiac specialist like Dr. Adam Budzikowski can provide the expertise and personalized care needed to determine the best treatment path.
CRR