Pulsed field ablation (PFA) is a groundbreaking advancement in arrhythmia treatment that offers precision and safety through targeted electrical pulses, minimizing damage to surrounding tissues.
Understanding Pulsed Field Ablation
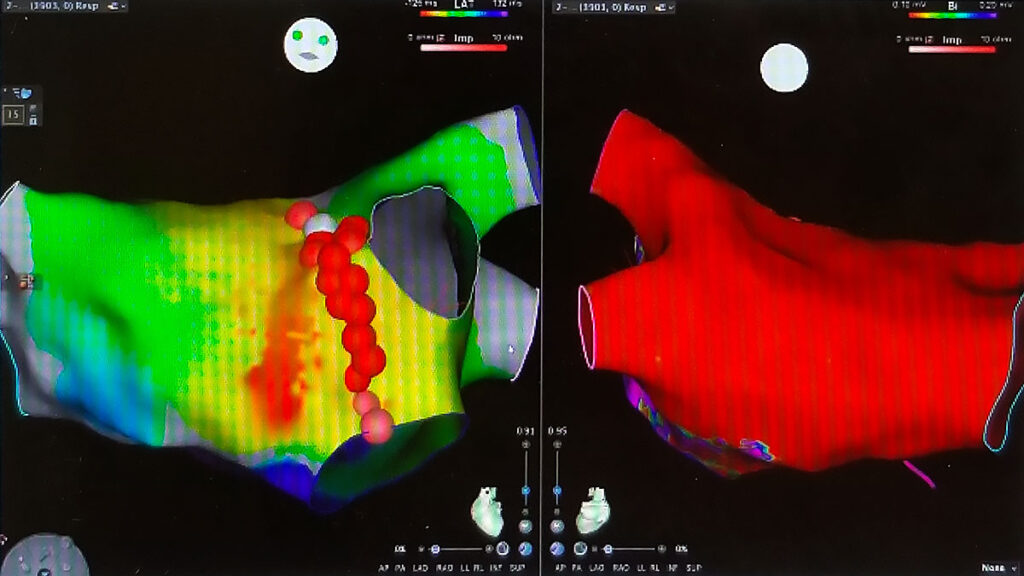
Pulsed field ablation (PFA) is an emerging technology in the treatment of cardiac arrhythmias, particularly atrial fibrillation (AFib). Unlike traditional thermal ablation methods, which use heat (radiofrequency) or extreme cold (cryoablation) to create lesions in the heart tissue, PFA employs high-voltage electrical pulses to selectively target cardiac cells while preserving surrounding structures. This technique offers the potential for greater precision and safety in arrhythmia treatment.
How Pulsed Field Ablation Works
PFA operates through a process called electroporation, in which brief but intense electrical pulses create microscopic pores in cell membranes. This selectively disrupts abnormal cardiac tissue without causing excessive damage to adjacent structures like the esophagus, phrenic nerve, or blood vessels. As a result, PFA may reduce the risk of complications commonly associated with traditional ablation techniques.
Key advantages of PFA include:
- Selective Targeting: PFA preferentially affects cardiac muscle cells while sparing non-cardiac tissues.
- Minimized Collateral Damage: The risk of injury to surrounding organs is significantly lower than with heat- or cold-based ablation.
- Shorter Procedure Times: PFA is often quicker to perform due to its efficient energy delivery system.
- Potential for Reduced Recurrence: Some studies suggest that PFA may offer long-term efficacy similar to or better than conventional ablation methods.
Clinical Applications of Pulsed Field Ablation
PFA is primarily being explored for the treatment of atrial fibrillation, the most common sustained arrhythmia worldwide. However, research is ongoing to evaluate its effectiveness for other arrhythmias, including ventricular tachycardia. The technique is particularly promising for patients who are at high risk of complications from conventional ablation procedures.
Recent clinical trials have demonstrated:
- High Success Rates: Early studies indicate that PFA achieves durable pulmonary vein isolation, a critical goal in AFib treatment.
- Reduced Risk of Thermal Injury: Unlike radiofrequency or cryoablation, PFA minimizes damage to adjacent tissues, lowering the risk of complications such as atrioesophageal fistula.
- Faster Recovery: Many patients undergoing PFA experience shorter recovery times and fewer post-procedural side effects.
Comparing Pulsed Field Ablation to Traditional Ablation Methods
While traditional ablation techniques like radiofrequency and cryoablation have been the standard for years, PFA presents a novel approach that could reshape arrhythmia treatment. Here’s how PFA differs from other methods:
- Energy Source: PFA uses high-voltage electrical pulses, while radiofrequency ablation relies on thermal heat and cryoablation on extreme cold.
- Target Selectivity: PFA has high specificity, affecting only cardiac cells and reducing unintended damage to surrounding structures. In contrast, radiofrequency ablation has a higher risk of affecting nearby tissues, and cryoablation has a moderate level of selectivity.
- Risk of Collateral Damage: PFA significantly reduces the risk of complications such as esophageal injury or phrenic nerve damage, which are more common with radiofrequency ablation. Cryoablation has a moderate risk profile.
- Procedure Time: PFA procedures are generally shorter compared to radiofrequency ablation, which takes longer, while cryoablation falls somewhere in between.
- Recovery Time: Patients undergoing PFA often experience a faster recovery compared to those treated with radiofrequency ablation, with cryoablation recovery times being moderate.
Impact on Pacemaker and ICD Implantations
One of the key considerations in arrhythmia treatment is whether a patient may require an implanted cardiac device, such as a pacemaker or implantable cardioverter-defibrillator (ICD). Pulsed field ablation (PFA) has the potential to influence these decisions by offering a highly selective approach to arrhythmia treatment. In some cases, effective PFA may reduce the need for long-term device implantation by restoring normal rhythm without permanent conduction system damage. However, for patients with underlying conduction system disease, pacemakers may still be necessary to maintain a stable heart rate following ablation.
For individuals at high risk of sudden cardiac arrest, PFA may be used in conjunction with an ICD to help manage arrhythmias more effectively. Additionally, as PFA evolves, it may be explored as a way to improve outcomes in patients already dependent on cardiac devices by reducing the burden of arrhythmias that necessitate frequent device therapy.
Limitations and Future Research
Despite its promising benefits, PFA is still undergoing clinical evaluation. Some of the challenges and considerations include:
- Limited Long-Term Data: While initial results are promising, more studies are needed to assess long-term efficacy and safety.
- Device Availability: PFA is not yet widely available and may take time to become a standard treatment option.
- Learning Curve: Physicians must undergo specialized training to adapt to this new technology effectively.
Future research aims to expand the use of PFA beyond atrial fibrillation, potentially applying it to ventricular arrhythmias and other complex cardiac conditions.
The Future of Pulsed Field Ablation
As more clinical trials confirm the safety and effectiveness of PFA, this technique has the potential to revolutionize arrhythmia treatment. With its ability to selectively target cardiac cells while minimizing risks, PFA may soon become the preferred method for many electrophysiologists.
If you have been diagnosed with atrial fibrillation or another arrhythmia, consulting a specialist is essential to determine the most suitable treatment. Dr. Adam Budzikowski specializes in advanced arrhythmia therapies, including the latest innovations in ablation techniques. Schedule a consultation today to explore your options.
A Riley Publication
Medically Reviewed By: Adam Budzikowski, MD, PhD